
Having started my consultant career at the Princess Royal Hospital in Telford I made a move across the region to Worcestershire for a combination of professional and personal reasons.
Covid had wreaked absolute havoc, and trying to rebuild clinical services during and after that was a tall ask. Getting back into the operating theatre and doing what I was employed to do was very difficult due to the changing needs of the region and the available capacity.
Trauma & Orthopaedics in particular suffered nationally and it has made me readjust my thinking about my specialty, and its place in the world.
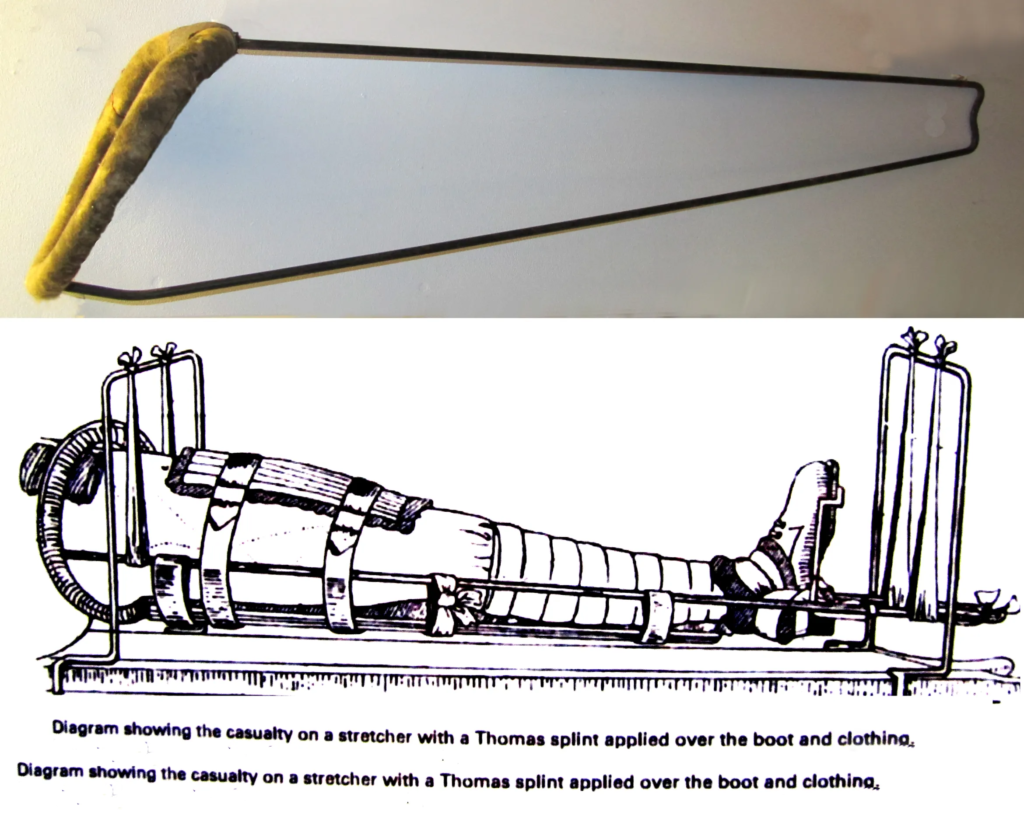
Trauma surgery is often life-saving. Without the advances that have been made in trauma care, mortality rates would be much higher. One of the best examples of this is still the Thomas Splint. First developed by Owen Thomas in the mid-1800’s it was popularised by Robert Jones during WW1 when its use reduced the mortality rate from open femoral fractures from 80% to 15%. For more information on the Thomas Splint click here
Joint replacement surgery isn’t really seen as life-saving but it is a quality of life surgery that aims to improve pain and secondarily improve function. The magnitude of the impact is evident when you see patients before and after surgery.
Before surgery it is about the desire to do the simple things. Getting a good nights rest, being able to cut down on or stop pain medication, or just being able to have a little walk outside. After surgery, it is so uplifting when patients start asking questions about what they can and can’t do. It’s no wonder that in terms of impact on physical and mental wellbeing Hip Replacement is seen as the ‘Operation of the Century’.
One of the biggest draws about coming to Worcestershire was the progress that had been made with the hot/cold split. This is essential for the delivery of non-emergency services. I’m fully aware that this has caused consternation within the community over the past decade or so, but in orthopaedics it is recognised that having a ‘cold site’ with a ring-fenced ward and dedicated theatres allows the delivery of increased volumes of surgery whilst minimising risks of complications, especially infection.
It is vital to know that joint replacement surgery is not just about the surgery. I tell every patient that it is a journey that includes preparation (including pre-hab), the surgery, the post-op recovery and rehabilitation. I’m fortunate to work with a tremendous team of anaesthetists, junior orthopaedic doctors, theatre staff, clinic and ward nurses, physiotherapists, occupational therapists and my administrative support who ensures that the right patients are in the right place at the right time.
So where am I now? I flew out of the blocks when I started at Telford and in the six months before COVID I was making solid progress through already busy waiting lists. With COVID and lockdown the service at Telford was suspended indefinitely. Moving to Worcester, I re-started immediately with the local backlog of cases and have the joy of working in a Trust where I know many of colleagues from my time as a trainee.
The support and forward thinking nature of the department has been great and when it comes down to it my first year at WorcsAcute has been excellent.
Onwards and Upwards…….
